Why Unmanaged Medical Devices Are a Growing Cyber Risk in Healthcare
 The Patient Safety Impact Most Cybersecurity Conversations Miss
The Patient Safety Impact Most Cybersecurity Conversations Miss
In May 2017, a ransomware attack disrupted healthcare delivery across the UK. In just 12 hours, more than 19,000 medical appointments were canceled, including 139 for suspected cancer patients. Emergency departments closed. Diagnostic equipment went offline. Care was delayed, not because clinicians lacked skill, but because medical devices were unavailable.
This incident remains a defining lesson for healthcare cybersecurity: when medical devices fail, patient care fails with them.
Fast forward to today, and the risk has only grown. Healthcare organizations rely on thousands of connected medical devices, many of which operate outside traditional IT visibility and patching workflows. These unmanaged devices have become one of the most dangerous, and least addressed, cyber blind spots in healthcare.
The Visibility Crisis in Healthcare Device Security
The scale of the problem is difficult to overstate.
According to 2025 research, 99% of healthcare organizations manage Internet of Medical Things (IoMT) devices with known exploited vulnerabilities, and 89% operate medical systems susceptible to publicly available exploits. Even more concerning, 96% of those vulnerabilities are linked to active ransomware campaigns.
Despite heavy investment in cybersecurity tools, many healthcare organizations still lack basic visibility into:
- What devices are connected
- Where they are located
- What operating systems they run
- What data they access or store
In many cases, the majority of unmanaged medical devices aren’t even registered with IT security teams.
Why Medical Devices Escape Traditional ITAM
Medical devices don’t behave like traditional IT assets, and healthcare organizations are structured in ways that unintentionally reinforce this gap.
Common reasons devices remain invisible include:
- Shadow IT in Clinical Environments
Medical devices are often introduced by clinical departments without formal IT approval. This includes imaging systems, diagnostic tools, department-managed EHR environments, and even smart devices brought in by staff. - Operational and Clinical Constraints
Many devices are purpose-built to perform a single clinical function and must operate 24/7. Downtime for patching or replacement can directly affect patient care. - Cross-Functional Ownership Gaps
Responsibility for medical devices is split across clinical engineering, biomedical teams, IT, procurement, and compliance – often without a single accountable owner.
The result is fragmented oversight, even in organizations with mature security programs.
Unsupported Operating Systems and the Patching Reality
One of the most persistent risks tied to unmanaged medical devices is outdated operating systems.
In 2025:
- 83% of medical imaging devices run outdated operating systems
- 70% of healthcare organizations worldwide still use outdated Windows systems
- Some hospitals continue to operate devices on Windows XP and Windows Server 2003, which are fully unsupported
Medical equipment can remain clinically effective for 10-20 years, far outlasting the lifecycle of the software it runs on. Replacing a CT scanner or MRI can cost millions of dollars, making software upgrades operationally and financially complex.
Why Patching Is “Incredibly Difficult”
Unlike SaaS platforms, medical device patching often requires:
- Physical technician visits
- Calibration and validation testing
- Temporary device removal from service
Healthcare technology managers must balance cybersecurity risk against patient safety and continuity of care. As a result, some devices inevitably slip through the cracks, leaving vulnerabilities unaddressed.
Compliance and Incident Reporting Consequences
Medical devices routinely generate, transmit, and store protected health information (PHI), including diagnostic results, treatment data, and usage records.
Under HIPAA, healthcare organizations must comply with three core requirements:
- Privacy Rule: Protecting PHI and patient rights
- Security Rule: Administrative, physical, and technical safeguards
- Breach Notification Rule: Mandatory reporting within defined timelines
Key compliance realities include:
- Affected individuals must be notified within 60 days of breach discovery
- Breaches affecting 500+ individuals require immediate reporting to HHS and regional media
- Non-compliance penalties can reach $50,000 per violation, with annual caps up to $1.5 million
Unmanaged devices complicate investigations, delay reporting, and increase regulatory exposure, especially when device details are missing or undocumented.
Why Asset Visibility Must Come First
You can’t protect what you can’t see.
Before healthcare organizations can apply security controls, they must first identify:
- Every connected medical device
- Its operating system and firmware
- Its communication patterns
- Its data exposure risk
A comprehensive medical device inventory enables:
- Risk prioritization
- Behavioral baselines for anomaly detection
- Faster incident response
- Improved audit readiness
Organizations with strong asset visibility also gain operational benefits, reducing unnecessary equipment purchases, improving device availability, and enabling faster patient care.
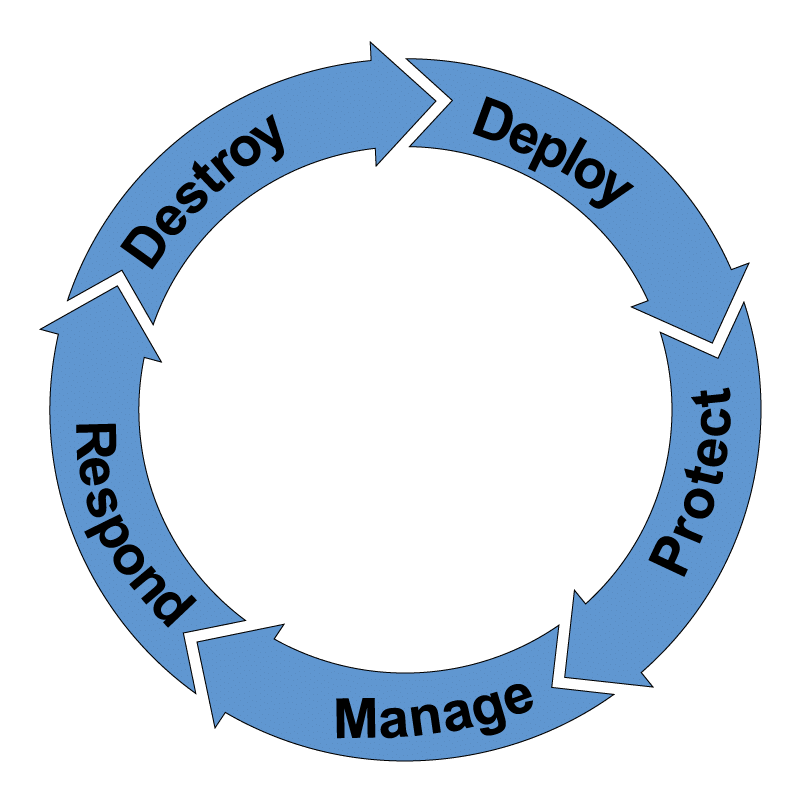
The Path Forward for Healthcare Leaders: Understand Your External Cyber Exposure
This is not a problem healthcare organizations can patch their way out of, and it’s not the result of negligence.
It’s a visibility and lifecycle management challenge.
Healthcare leaders should start with:
- A comprehensive medical device inventory
- Cross-functional coordination between IT, clinical engineering, and compliance
- Clear ownership and lifecycle accountability
- Secure disposition of retired devices containing PHI
Resilience360 gives healthcare leaders a clear, external view of cyber exposure, trust gaps, and visibility challenges without disrupting clinical operations.
In a 30-45 minute executive session, we’ll help you understand where risk exists today and what to prioritize next to strengthen cyber resilience.